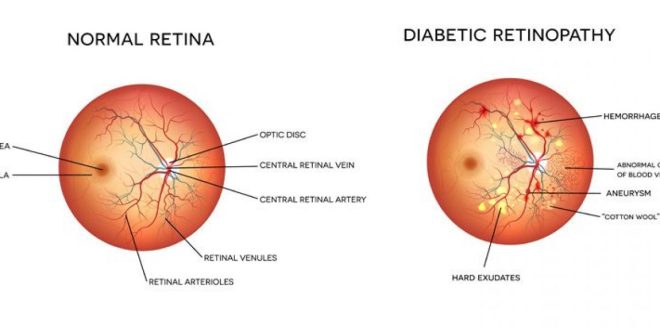
Diabetic retinopathy (die-uh-BET-ik retin-NOP-uh-thee), is an eye-related consequence of diabetes. The blood vessels of the light-sensitive tissue in the back of the eye are damaged, which is what causes it (retina).
The early stages of diabetic retinopathy may show no symptoms or very minor vision issues. However, it may result in blindness.
Diabetes Eye Disease: The Two Stages
Diabetic eye disease progresses through two primary stages.
NPDR (non-proliferative diabetic retinopathy)
Diabetic eye disease is currently in its early stages. Diabetes affects a large number of people.
Tiny blood vessels leak in NPDR, inducing swelling of the retina. Macular edoema refers to the swelling of the macula. The most typical cause of visual loss in diabetic patients is this.
Additionally, blood vessels in the retina may collapse with NPDR. We refer to this as macular ischemia. Blood cannot enter the macula in that situation. In the retina, small specks known as exudates can occasionally occur. Your vision may be impacted by these.
Your eyesight will be hazy if you have NPDR
PDR (proliferative diabetic retinopathy)
PDR is the later stage of diabetic retinopathy. It occurs when the retina begins to produce new blood vessels. The term for this is neovascularization. Frequently, the vitreous leaks into these tender young vessels. You might notice a few dark floaters if they bleed just a little bit. A lot of bleeding could completely impair vision.
Risk factors & causes
The damage that diabetes does to the tiny blood vessels in the retina leads to diabetic retinopathy. Vision loss can result from these damaged blood vessels:
- The region of the retina that is responsible for sharp central vision, the macula, might experience fluid leakage. The macula, a tiny portion of the retina, is what gives humans the ability to see colour and fine detail. Blurred results from the fluid swelling the macula.
- New blood vessels might develop on the retina’s surface in an effort to enhance blood flow there. These weak, aberrant blood vessels may rupture and leak blood into the back of the eye, impairing vision.
Diabetes’s effects on the eyes
The layer of light-sensitive cells in the back of the eye called the retina is responsible for converting light into electrical signals. Sending the signals to the brain causes it to transform them into the visuals you see.
The retina requires a steady flow of blood, which it gets via a web of small blood vessels.
A chronically high blood sugar level can harm these blood vessels over time in three primary stages:
- Background retinopathy: Tiny blood vessel bulges that may slightly bleed but typically do not impair vision occur.
- Pre-proliferative retinopathy: More extensive and pervasive alterations to the blood vessels, including increased eye bleeding
- Proliferative retinopathy causes the retina to generate scar tissue and new, weak blood vessels that bleed easily. This can cause some vision loss.
However, if an issue with your eyes is identified early, lifestyle modifications and treatment can prevent it from getting worse
Scar tissue may be created by these new blood vessels. The macula may experience issues or develop a detached retina as a result of scar tissue.
Stages
The four stages of diabetic retinopathy are as follows:
- Nonproliferative mild retinopathy. Your retina’s small blood vessels change in the early stages of the disease. Smaller regions swell. They are known as microaneurysms. Your retina may be affected by fluid leakage from them.
- Moderate nonproliferative retinopathy. Blood vessels that ought to maintain the health of your retina swell and alter shape as your condition worsens. They are unable to bring blood to your retina. This may alter how your retina appears. Diabetic macular edoema may result from these alterations in the blood vessels (DME). The macula, a portion of your retina, is swollen.
- Severe nonproliferative retinopathy. The third stage sees the blockage of numerous blood arteries. They are unable to provide blood to your retina to maintain its health.
Where this occurs in your retina, special proteins called growth factors are produced. These proteins instruct your retina to develop new blood vessels.
- Proliferative diabetic retinopathy (PDR). The most advanced stage is this one. Your retina and the vitreous humour, a jelly inside your eyeballs, both experience new blood vessel growth. It is more common for fragile young blood vessels to haemorrhage and leak liquids. Scar tissue begins to develop. Your retina may tear away from the tissue beneath as a result, leading to retinal detachment. Permanent blindness may result from this.
Is diabetic retinopathy curable?
However, each stage of diabetic retinopathy can be handled differently. Laser surgery is frequently used to treat diabetic eye disease.
Background retinopathy is incurable, but patients must undergo routine eye exams.
Typically, laser therapy is used to treat maculopathy (tiny burns that help to prevent new blood vessel growth and improve the nutrient and oxygen supply to the retina). Although typically painless and without any negative side effects, this can affect night driving and peripheral vision.
Though it won’t enhance vision, this kind of laser therapy for diabetic retinopathy can stop it from getting worse. With a scattering of lasers across the entire retina, proliferative retinopathy is also treated.
Can diabetes-related retinopathy be prevented?
There are steps you may take to lower the risk of diabetic retinopathy developing or worsening, despite the fact that prevention of it can be difficult.
Every year, have your eyes checked for diabetes
An eye exam can assist in the diagnosis of eye conditions that require treatment and can inform you and our best eye specialist in west delhi if your diabetes needs to be better managed. Before becoming pregnant or during the first trimester, women with diabetes should get an eye checkup. Depending on the severity of the retinopathy, continue to be checked throughout each trimester and for a year after birth.
Follow your diabetes management plan
To get the most out of your therapy, follow these instructions:
- As directed, take your medications.
- If needed, provide insulin as prescribed.
- To control blood sugar levels, eat a healthy, balanced diet.
- Exercise will lower blood sugar levels and aid the body’s utilisation of them.
- Regularly check your blood sugar levels.
- Check your haemoglobin A1c levels frequently.
- Maintain a regular urine ketone test.
- Maintain regular follow-ups with your doctor to assess your diabetes management and to rule out or treat any other risk factors, such as high blood pressure.
Also Read:
 Posting Point
Posting Point